ARE CANCER DRUGS THE SOLUTION TO ALZHEIMER'S DISEASE?
USING CANCER DRUGS TO TREAT NEURODEGENERATION.
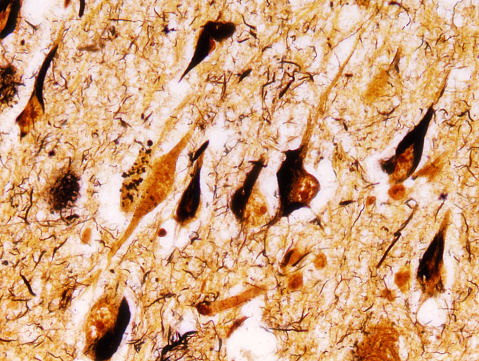
Title image shows Neurofibrillary tangles in Alzheimer's Disease brain.
Last August, former President Jimmy Carter announced that the melanoma that was first found in his liver had spread to his brain. His prognosis was poor, but by December of the same year, he announced that he was cancer free. He attributes his recovery to use of the new cancer drug, pembrolizumab. However, a recent publication by Baruch, et al. in Nature Medicine suggests that this drug may not only be a miracle for cancer patients, but also for the 5.2 million Americans suffering from Alzheimer’s Disease as well.
Pembrolizumab, also known by the brand name Keytruda, is one of several new tumor immunotherapy drugs classified as a checkpoint inhibitor. Rather than killing cancer cells, these drugs block the natural inhibitory signals (or “checkpoints”) on immune cells, thus pulling the brakes off of the immune system and allowing it to fight cancer cells more effectively. This drug in particular is an antibody that targets PD-1, a protein responsible for transmitting inhibitory signals to immune cells. By blocking these signals, pembrolizumab permits immune cells to maintain their activation status and attack tumor cells.
Modulating the immune system is not just a therapeutic approach for combating cancer, though. The importance of a strong immune system for fighting infections has long been known, as has the importance of suppressing the immune system in cases such as autoimmunity. Additionally, scientists have recently begun exploring the role that the immune system plays in neurodegenerative diseases such as Alzheimer’s Disease and Parkinson’s Disease.
Alzheimer’s Disease is one of the most common diseases in the United States, affecting 1 in 9 people over the age of 65 and 1 in 3 people over the age of 85. Patients with the condition may suffer from memory loss, confusion, difficulties solving problems or communicating, and changes in mood and personality. While many existing drugs may help slow the progression of the disease, none can stop it or reverse the damage that it has already done. In order to design more effective treatment options, scientists are currently studying the mechanisms by which Alzheimer’s Disease arises and causes symptoms.
Alzheimer’s Disease, like many neurodegenerative diseases, is associated with the deposition of misfolded proteins throughout the brain. In Alzheimer’s Disease, the misfolded protein of interest is known as amyloid beta, and it not only interferes with the brain’s ability to function, but its presence may also cause more misfolded protein to be deposited, resulting in the worsening of symptoms over time. A healthy immune system responds to these proteins by clearing them up before any disease can occur. Specifically, phagocytic immune cells such as macrophages and microglia eat and degrade these proteins. However, when phagocytes fail to clear up misfolded amyloid beta, Alzheimer’s Disease can progress. While it is unclear why the immune system sometimes fails to clear amyloid beta, scientists have started investigating whether activating the immune system can alleviate symptoms of Alzheimer’s Disease by encouraging phagocytes to eat more of the misfolded protein.
In their recent Nature Medicine paper, Baruch, et al. questioned whether checkpoint inhibitors could help eliminate amyloid beta in Alzheimer’s Disease the same way that they help eliminate tumor cells—by pulling the brakes off of the immune system. In order to address this question, they took advantage of a mouse model of Alzheimer’s Disease in which mice have a gene mutation previously shown to participate in the pathogenesis of Alzheimer’s Disease in both mice and humans2. They treated these mice with an anti-PD-1 antibody, very much like pembrolizumab, and found that doing so was sufficient to induce the production of a pro-inflammatory molecule known as interferon gamma (IFNg). They also observed that treatment with the anti-PD-1 antibody caused phagocytes to migrate to the brain. When IFNg was blocked, the phagocytes failed to enter the brain. Once in the brain, the phagocytes were capable of clearing amyloid beta, and mice treated with the anti-PD-1 antibody also performed better than control mice on a cognitive and memory test, suggesting an improvement in symptoms associated with Alzheimer’s Disease. In fact, treated mice performed almost as well on these tests as healthy mice, indicating an almost complete reversal of the disease.
So is pembrolizumab the next miracle drug? Can it cure both cancer and Alzheimer’s Disease? Don’t get your hopes up quite yet. While pembrolizumab has proven effective in many cancer patients like Jimmy Carter, it doesn’t work for everybody, and it doesn’t work for all types of cancer. Furthermore, its efficacy as a treatment for Alzheimer’s Disease is all but proven. In their study, Baruch, et al. noted that Alzheimer’s symptoms returned after stopping treatment2, so an anti-PD-1 antibody would likely be a treatment option, not a cure. Furthermore, other studies have also demonstrated the efficacy of immunotherapies in the treatment of neurodegenerative diseases only to fail in a clinical setting. Notably, many of these immunotherapies actually sought to suppress the immune system, as it has also been shown that activated immune cells in the brain can actually worsen neurodegenerative diseases in some cases. So whether the ideal treatment for neurodegenerative diseases works by activating or suppressing the immune system is still up in the air.
There is still hope yet, though, as several novel immunotherapies are proving efficacious in the treatment of Alzheimer’s Disease. Three antibodies (solanezumab, gantenerumab, and aducanumab) that bind to different parts of misfolded amyloid beta fibrils are currently undergoing clinical trials. While solanezumab and gantenerumab have mostly shown beneficial in patients treated early, aducanumab was the first to show significant clearance of amyloid beta in the brain3.
If scientists can design a drug that effectively clears amyloid beta from the brain, they will pave the way for new treatments not only for Alzheimer’s Disease, but also for other neurodegenerative diseases as well. Because many neurodegenerative diseases are associated with the deposition of misfolded proteins, it is possible that designing antibodies to target the protein of interest in each disease will prove efficacious. Further, it is possible that pulling the brakes off of the immune system with checkpoint inhibitors may be effective at clearing not only amyloid beta, but also other misfolded proteins as well. Given that cancer and neurodegenerative diseases frequently occur in older patients, a single treatment option for both would be remarkably beneficial. So, if checkpoint inhibitors prove efficacious in the treatment of Alzheimer’s Disease, and potentially other neurodegenerative diseases as well, they may truly be the miracle drug.
REFERENCES
2015 Alzheimer’s Disease Facts and Figures. Alzheimer’s Association. [http://www.alz.org/facts/downloads/facts_figures_2015.pdf]
Baruch, et al. “PD-1 immune checkpoint blockade reduces pathology and improves memory in mouse models of Alzheimer’s disease.” Nature Med 22(2) 2016.
Frantz, Niles. “Clinical Trials Results and New Data Analyses in Amyloid-Related Therapies from the Alzheimer’s Association International Conference 2015.” Alzheimer’s Association July 22, 2015.