FOOD ALLERGIES: ITCHING FOR PREVENTION
NEW RESEARCH SUGGESTS ALLERGIES CAN BE PREVENTED RATHER THAN JUST TREATED.
When my brother was very young, he found a peanut butter cookie on the ground while he was following my mom in the grocery store, and he picked it up. When my mom noticed a few minutes later, my brother’s hands were bright red and had started to itch. She quickly took the cookie from him and gave him an antihistamine to stop the swelling and itching. If she hadn’t noticed in time and he had eaten some of the cookie, he could have suffered a severe allergic reaction.
Growing up with food allergies is not easy, and it’s becoming a problem more and more children are facing. For my little brother, it meant following a strict diet prohibiting eggs, dairy, and nuts. All of the food in our house was labeled with big red and green stickers: red meaning the food was “itchy” and green meaning it was safe for him to eat. He had to sit at a separate peanut-free table for lunch at his elementary school and carry around his EpiPen wherever he went (he still does this today at age 15).
In 1996, before my brother was born, only 0.4% of US children had peanut allergies, but by 2008, that number was up to 1.4% (1). The total number of children in the US with any type of food allergy is now as high as 8% (1). There are many theories for why the number of children with food allergies is increasing, but none of these theories have been proven true. Most children with allergies to dairy, eggs, wheat, and soy will outgrow their allergies by the time they reach adulthood, but most children with nut, fish, and shellfish allergies will not. As the number of children with food allergies continues to increase, it is becoming more and more clear that emergency medication and treatment after an allergy attack is not the best solution to treating allergies (and neither is Louis C.K.’s “but maybe” solution – this is one of my family’s favorite stand-up comedy routines).
Allergy attacks are caused by an immune reaction. Your immune system normally attacks invading bacteria or viruses to keep you healthy. In a child with food allergies, the immune system recognizes certain types of food as dangerous to the body (even though they shouldn’t be) and will try to attack those food particles, resulting in swelling and an itchy feeling. Thus, most of current food allergy research is focused on controlling this inappropriate immune reaction through immunotherapies.
The idea behind immunotherapy is that if you start giving a child very small quantities of an allergen, and then slowly increase the amount over time, eventually the body will learn to tolerate the allergen. There are two main types: oral, in which small amounts of the allergen are mixed with other food and eaten, and sublingual, in which small drops of the allergen are administered under the tongue (1). While these therapies have decreased allergic reactions to trace amounts of allergens in clinical trials, they are not a cure. Many of the patients can still only tolerate small amounts of the allergen. The treatments are costly and must occur over many months. Might there be a way to prevent allergies from developing in the first place?
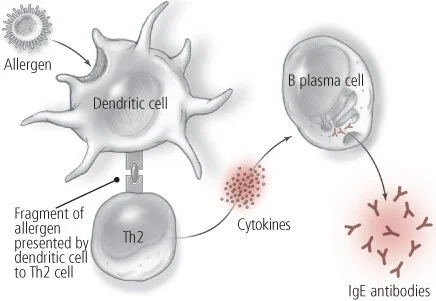
Based on a recently published article by Zhang, et al. (2), it seems like that may one day be an option. From previous studies, we know that the first time an allergic reaction occurs, immune system cells called dendritic cells recognize the allergen as foreign. They break down the allergen and show a piece of it to another type of immune cell called a T helper 2 (Th2) cell, which sends out signals (called cytokines) to the body to produce an immune reaction (Figure 1). After the first allergic reaction, the body’s immune system has a memory of the allergen, so it responds more quickly. However, it was not well understood why this first allergic reaction occurs in some people but not in others. Zhang and her colleagues thought the answer might lie in what an individual’s immune system is like at birth.
In their study, Zhang, et al., examined the immune properties of the cord blood of a group of infants, and tested the infants at 1 year to determine whether or not they had developed food allergies. The authors found that the infants who later developed food allergies had a greater number of inflammation-producing immune cells than infants who did not have food allergies. The authors also found that these cells were more sensitive, meaning the cells produced more inflammation signals when they saw something they recognized as dangerous to the body. These inflammatory signals cause greater production of Th2 cells, the cells that are responsible for signaling an allergic reaction, in the infants with food allergies than in those without. From these observations, Zhang, et al., concluded that the higher number of sensitive inflammation-producing immune cells in infants who developed food allergies may be the source of their initial reactions to food allergens.
What does this mean? If we could test infants early on to see how much inflammation their immune systems produce, we could identify which of the infants would develop food allergies and potentially treat them to decrease the overproduction of these inflammatory signals. Perhaps this would decrease the number of the Th2 cells that are produced so that the risk of reaction to food is reduced. What hurdles still remain for such a treatment to become a reality?
The important next step for researchers would be to identify a molecule or pathway in our bodies that can reduce the amount of inflammation natively in someone’s immune system. However, even if researchers find a way to reduce this inflammation, it must first be thoroughly tested both in animals and in human cells cultured outside the body. If these tests showed that the treatment was effective and didn’t have any side effects, the treatment still must go through clinical trials before the FDA would approve it for widespread use. While this idea would need a lot more testing before we could try to use this information to treat humans, it makes me hopeful that a way to prevent food allergies from developing may one day be a possibility.
REFERENCES
Le, U.H., & Burks, A.W. (2014). Oral and sublingual immunotherapy for food allergy. World Allergy Organization Journal, 7(35). [http://www.waojournal.org/content/7/1/35].
Zhang, Y., et al. (2016). Cord blood monocyte–derived inflammatory cytokines suppress IL-2 and induce nonclassic “TH2-type” immunity associated with development of food allergy. Science Translational Medicine 8(321). [http://stm.sciencemag.org/content/8/321/321ra8]