THE GUT-BRAIN AXIS AND ITS ROLE IN PARKINSON’S DISEASE
CAN WE TREAT OR PREVENT NEUROLOGICAL DISEASE BY MANIPULATING BUGS IN OUR GUT?
After we eat a meal, we feel full, which triggers us to stop eating. This critical phenomenon is due to communication between the gut and the brain. Intriguingly, it is increasingly clear that communication between the gut and the brain occurs in a wide variety of situations, not limited to those related to food. This communication is called the “gut-brain axis” and is a rapidly accelerating field of research.
gutmicrobiotaforhealth.com
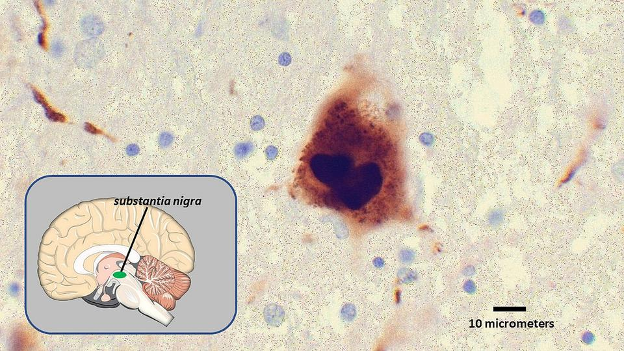
Understanding the gut-brain axis is important because it may help us find new treatments for devastating neurological diseases. For example, there is great interest in understanding how the gut-brain axis may drive or worsen Parkinson’s disease, an age-related neurological disorder that affects at least 10 million individuals across the globe. Patients with Parkinson’s disease have trouble with their movements and may also ultimately develop memory impairments or other cognitive symptoms. Additionally, the brains of patients with Parkinson’s disease look different than healthy brains. Parkinson’s brains tend to have abnormal and large clumps of a molecule called alpha-synuclein. These clumps are likely toxic, as their presence is linked to abnormal functioning of neurons.
hopkinsmedicine.org
Clump of abnormally structured alpha synuclein in the brain of a Parkinson’s patient. This clump was found in the substantia nigra, a brain region involved in movement.
Sadly, the prevalence of Parkinson’s disease is only expected to increase as the human lifespan increases. Treatments are currently available, primarily in the form of pills or a procedure called deep brain stimulation. Unfortunately, deep brain stimulation is invasive, and the current pills are not effective for all patients. In addition, they tend to wane in effectiveness over time. Therefore, novel approaches are desperately required.
Medications targeting the gut, rather than the brain, would be highly novel. One reason that scientists are interested in this angle is that gastrointestinal issues are strongly linked to the development of Parkinson’s disease. For example, constipation increases the risk of Parkinson’s disease up to 4x. Inflammatory bowel disease also increases risk. Gastrointestinal issues are also a symptom of Parkinson’s disease; up to 90% of Parkinson’s patients experience constipation alone.
Despite the strong ties between gastrointestinal dysfunction and Parkinson’s disease, it is unclear whether “gut issues” actually cause or worsen Parkinson’s disease. However, recent research suggests that this is likely. One relevant scientific discovery is described below.
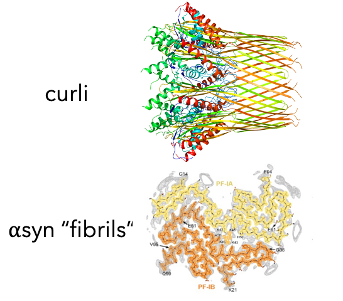
As a relevant context for the discovery, the gut is a crowded environment, teeming with trillions of microbes. These microbes produce many molecules that can cause effects on human cells. For example, a molecule called butyrate serves as energy for human cells that line the intestine. Relevant to Parkinson’s disease, one microbe produces a molecule called curli, which resembles the clumps of alpha-synuclein found in the brains of Parkinson’s patients.
(top) from Willyard, Nature 2021; (bottom) Tau2020 Global Conference
Scientists hypothesized that feeding the microbe producing curli to mice might prompt or accelerate Parkinson’s-like symptoms. Indeed, this is exactly what happened. After being provided with the microbe, the mice experienced a decline in their motor abilities. Though it is unclear how curli may have caused this effect, it is possible that it traveled from the gut to the brain via a pathway called the vagus nerve, where it then served as a template for alpha-synuclein to aggregate and cause harmful brain toxicity.
There are many questions left to answer - most importantly, can microbe-based treatments be used to treat or prevent Parkinson’s disease? Excitingly, these treatments would likely be very accessible, as they would likely come in the form of a pill. Though we are years away from being able to answer this question, investigations of the gut-brain axis may well transform medical understanding of how to treat neurological disease, and thus improve quality of life for millions of patients and their caregivers.
REFERENCES
https://www.parkinson.org/Understanding-Parkinsons/Statistics
https://www.mayoclinic.org/diseases-conditions/parkinsons-disease/diagnosis-treatment/drc-20376062
https://www.sciencedirect.com/science/article/pii/S1353802014003630
https://academic.oup.com/ibdjournal/article/25/1/111/4996912
https://www.sciencedirect.com/science/article/pii/S1474442215000071?via%3Dihub#tbl1